DISCLAIMER
The content provided in this Substack post is for entertainment and informational purposes only and is not intended to serve as medical advice. The views and opinions expressed herein are those of the writer and should not be taken as definitive or authoritative. Readers should not rely solely on the information provided in this post to make decisions about patient care. Instead, use this content as a starting point for further research and consult a qualified healthcare professional before making any changes to treatment or medication regimens.
Antipsychotic medications are an essential part of the treatment of various mental health disorders, including schizophrenia and bipolar disorder. However, not all antipsychotic medications are created equal, and sometimes it becomes necessary to switch from one medication to another. The process of switching from one antipsychotic to another can be simple or can be complex, and the method of switching can depend on several factors, including the risk of cholinergic rebound.
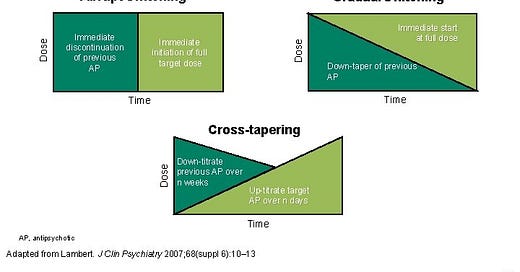
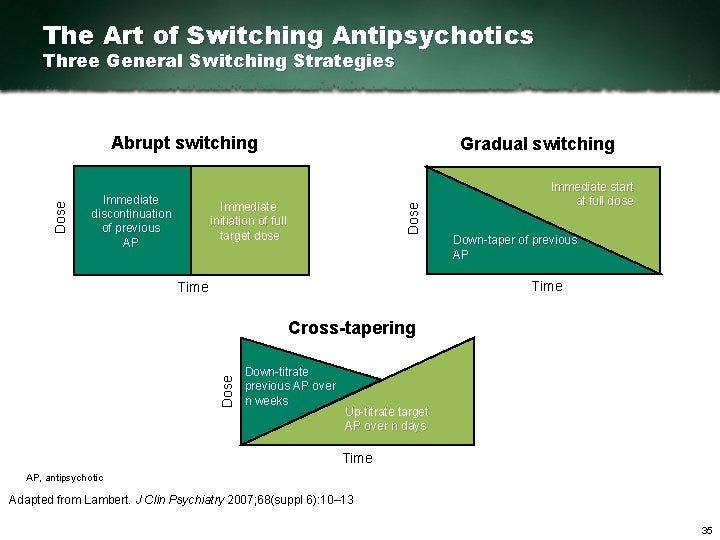
While it is true that you could probably get by skipping this post and simply referring to this tool. It is unbecoming of an individual who is seeking mastery in a field to be wholly reliant on a resource such as that. With that said, it is a great resource to utilize & probably ought to be utilized until you are confident in your ability to switch antipsychotics safely. There is no honor in doing things our own way, when there is a right way after all. There are many other online resources discussing the general strategies surrounding switching antipsychotics, which are depicted in the graphic below.
Okay… back to the topic of *this* post. What is cholinergic rebound anyways?
Cholinergic rebound is a phenomenon that can occur when certain antipsychotic medications, particularly those with strong anticholinergic properties, are abruptly discontinued. Symptoms of cholinergic rebound can include the following: sialorrhea, nausea, vomiting, diarrhea, headaches, dizziness, agitation, confusion, delirium, and even seizures. Because of this, it is essential to consider the risk of cholinergic rebound when deciding whether to cross-taper or immediately switch antipsychotics.
When switching from one antipsychotic to another, PMHNPs should evaluate several factors, including the patient's current symptoms, medical history, and potential adverse effects of the medications. PMHNPs should also assess the risk of cholinergic rebound, particularly when the current medication has strong anticholinergic properties.
In cases where the current medication has a high risk of cholinergic rebound, PMHNPs may choose to cross-taper the medication rather than immediately switching. Cross-tapering involves gradually reducing the dose of the current medication while simultaneously increasing the dose of the new medication. This approach can minimize the risk of cholinergic rebound and other adverse effects that may occur with abrupt discontinuation.
On the other hand, in cases where the risk of cholinergic rebound is low, PMHNPs may choose to immediately switch the medication. This approach involves stopping the current medication and starting the new medication at the recommended dose. This approach can be appropriate when the patient's symptoms are severe, the current medication is not effective, or the medication is causing significant adverse effects.
With that said, I’ve included lists of antipsychotic medications that are considered to have high anticholinergic effects as well as low anticholinergic effects. If switching from one medication on the high list to another on the high list, then the risk of cholinergic rebound is obviously reduced. Another way of conceptualizing which medications have high anticholinergic effects is to think of which antipsychotics have low potency. High potency antipsychotics generally have a higher affinity for dopamine receptors compared to muscarinic receptors.
Antipsychotics which have high anticholinergic effect:
Clozapine (Clozaril)
Olanzapine (Zyprexa)
Quetiapine (Seroquel)
Chlorpromazine (Thorazine)
Thioridazine (Mellaril)
Fluphenazine (Prolixin)
Trifluoperazine (Stelazine)
Perphenazine (Trilafon)
Promethazine (Phenergan)
Antipsychotics which have low anticholinergic effect:
Here is a list of some antipsychotic medications with low anticholinergic effects:
Aripiprazole (Abilify)
Lurasidone (Latuda)
Asenapine (Saphris)
Ziprasidone (Geodon)
Risperidone (Risperdal)
Paliperidone (Invega)
Iloperidone (Fanapt)
Molindone (Moban)
It is essential to note that the degree of anticholinergic effects can vary from person to person, and not all individuals may experience cholinergic rebound when stopping these medications. Nonetheless, PMHNPs should carefully evaluate the risk of cholinergic rebound when considering switching from these medications to another antipsychotic medication.
There are other factors to consider when switching antipsychotics. Some of which will be discussed in future posts.
DISCLAIMER
This is not Medical Advice and while the writer believes what he has shared, substack dot com does not equate to strong evidence. Please do not treat patients based on what is read in this post, these are opinions of an internet stranger. Instead use these posts as a starting point for furthering your own study & education.