How to Write a Soap Note
(For students)
DISCLAIMER
The content provided in this Substack post is for entertainment and informational purposes only and is not intended to serve as medical advice. The views and opinions expressed herein are those of the writer and should not be taken as definitive or authoritative. Readers should not rely solely on the information provided in this post to make decisions about patient care. Instead, use this content as a starting point for further research and consult a qualified healthcare professional before making any changes to treatment or medication regimens.
Introduction:
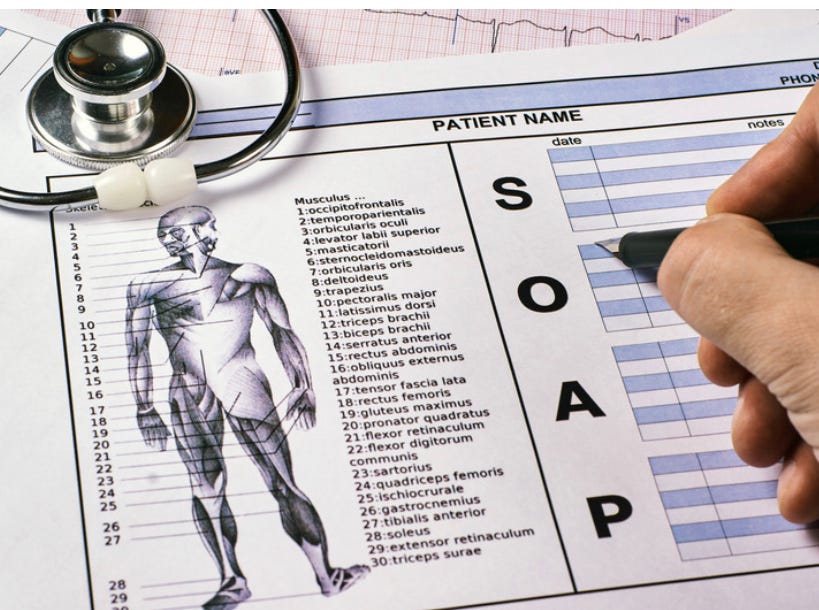
SOAP (Subjective, Objective, Assessment, and Plan) notes are a structured method for documenting patient information and creating a treatment plan in psychiatric mental health nurse practice. This guide provides a thorough overview of SOAP notes, their purpose, and essential elements tailored for PMHNPs. By following these steps, you will be well-equipped to write clear and effective SOAP notes.
Section 1: Overview of SOAP Note Components
Subjective: Patient-reported information, including chief complaint and history
Objective: Clinician-observed data, such as mental status exam findings
Assessment: A summary of the patient's psychiatric condition and potential diagnoses
Plan: Treatment and management strategies for the patient's psychiatric condition
Section 2; The Subjective (S) Component Includes:
Chief complaint (CC): The primary reason for the patient's visit, in their own words, related to their mental health concerns
History of present illness (HPI): A detailed description of the patient's symptoms, including onset, duration, severity, and any aggravating or alleviating factors
Past psychiatric history (PPH): A summary of the patient's previous mental health issues, treatments, and hospitalizations
Past medical history (PMH): A summary of the patient's previous medical issues, surgeries, allergies, and current medications
Family history (FH): Relevant mental health conditions affecting the patient's immediate family members
Social history (SH): Information about the patient's lifestyle, including occupation, living situation, relationships, smoking, alcohol, and drug use
Sample Subjective:
CC: "I've been feeling extremely sad and hopeless for the past month."
HPI: The patient reports a gradual onset of depressive symptoms, starting approximately one month ago. Symptoms include persistent low mood, loss of interest in previously enjoyed activities, insomnia, fatigue, and feelings of worthlessness. The patient denies any suicidal ideation or plan but feels hopeless about the future. No recent stressors or triggers identified.
PPH: The patient was diagnosed with major depressive disorder five years ago and had a prior hospitalization for a suicide attempt three years ago. Successfully completed a course of cognitive-behavioral therapy two years ago.
PMH: Hypothyroidism, well-controlled with levothyroxine
FH: Mother had a history of depression; brother has bipolar disorder
SH: Single, lives alone, employed as a teacher, denies smoking, occasional alcohol use, and no illicit drug use
Section 3; The Objective (O) Component Includes:
Mental status exam (MSE): A systematic assessment of the patient's appearance, behavior, speech, mood, affect, thought process, thought content, perception, cognition, and insight
Any relevant physical examination findings
Results from laboratory tests or imaging studies, if applicable
Sample Objective:
MSE: The patient is well-groomed and appropriately dressed. Cooperative and maintains good eye contact. Speech is slow and low in volume. Mood is reported as "depressed," with a congruent, restricted affect. Thought process is linear and goal-directed. Thought content reveals no suicidal or homicidal ideation, delusions, or hallucinations. Attention and concentration are intact. Memory and orientation are within normal limits. Insight and judgment are fair.
Section 4; The Assessment (A) Component Includes:
Summarize the patient's psychiatric condition based on the information gathered in the Subjective and Objective sections
Formulate a list of potential diagnoses or differential diagnoses, prioritizing the most likely diagnosis based on the collected data
Include any relevant diagnostic codes (e.g., from the DSM-5)
Sample Assessment:
The patient presents with a one-month history of depressive symptoms, including low mood, anhedonia, insomnia, fatigue, and feelings of worthlessness. Based on the patient's history and mental status exam findings, the primary diagnosis is:
Major Depressive Disorder, recurrent, moderate
Section 5; Writing the Plan (P) Component:
Outline the treatment and management strategies for the patient's psychiatric condition, considering both pharmacological and non-pharmacological interventions
Include any diagnostic tests, medications, therapy referrals, patient education, and follow-up appointments
Consider the patient's preferences and any contraindications when creating the treatment plan
Sample Plan:
Laboratory tests: Order a complete blood count (CBC), comprehensive metabolic panel (CMP), and thyroid-stimulating hormone (TSH) to rule out any underlying medical conditions contributing to the depressive symptoms
Medications: Initiate sertraline 50 mg once daily for depression, with instructions to report any side effects or worsening symptoms to the PMHNP
Psychotherapy: Refer the patient to a therapist for cognitive-behavioral therapy (CBT) to address depressive symptoms and improve coping skills
Patient education: Educate the patient on the importance of medication adherence, potential side effects, and the benefits of therapy
Follow-up: Schedule a follow-up appointment in two weeks to assess the patient's response to treatment and adjust the plan as needed
Conclusion:
Writing effective SOAP notes is an essential skill for psychiatric mental health nurse practitioners to ensure accurate documentation, clear communication, and optimal patient care. By following this guide and tailoring it to your specific clinical setting and patient population, you can develop a thorough understanding of SOAP note components and create comprehensive and effective notes.