Xylazine in Illicit Fentanyl and Implications for PMHNPs
DISCLAIMER
The content provided in this Substack post is for entertainment and informational purposes only and is not intended to serve as medical advice. The views and opinions expressed herein are those of the writer and should not be taken as definitive or authoritative. Readers should not rely solely on the information provided in this post to make decisions about patient care. Instead, use this content as a starting point for further research and consult a qualified healthcare professional before making any changes to treatment or medication regimens.
Introduction:
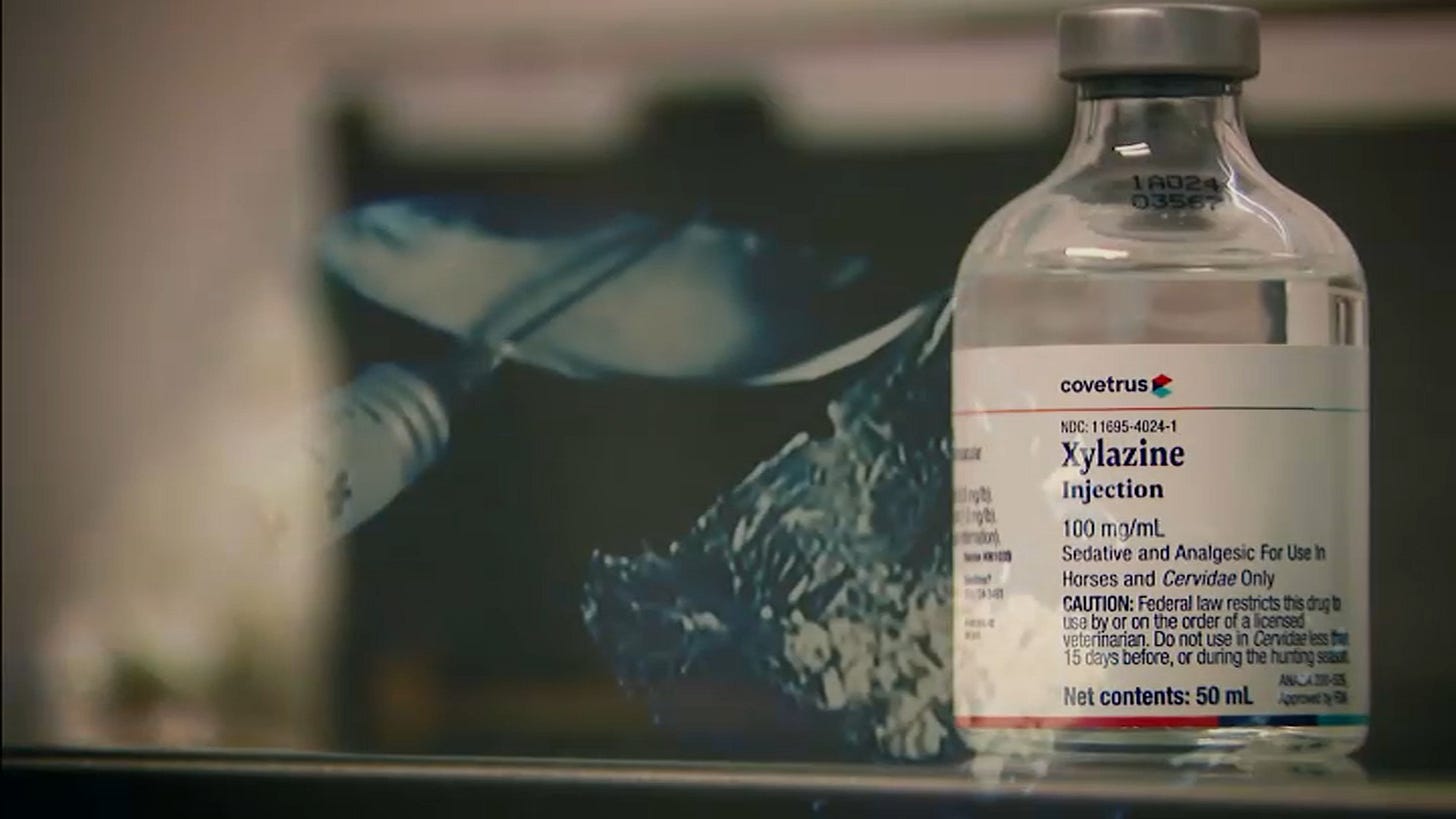
The landscapes of illicit drug use and opioid addiction are evolving, making the already arduous journey to recovery even more challenging. A recent phenomenon is the adulteration of illicit fentanyl with xylazine, a veterinary sedative. In other words, fentanyl is being laced with a horse tranquilizer. What could go wrong? Understanding the implications of this dangerous combination and how it affects detoxification strategies is crucial for healthcare providers engaged in treating opioid use disorders.
Understanding Xylazine and Its Effects:
What is Xylazine…? Xylazine is a non-opioid drug primarily used in veterinary medicine for its sedative, analgesic, and muscle relaxant properties. When misused by humans, it causes profound sedation and can lead to significant medical complications, such as respiratory depression, bradycardia, hypotension, and serious skin lesions. When combined with potent opioids like fentanyl, the risk of severe complications, including overdose and death, is drastically amplified.
The Rise of Xylazine in Illicit Drug Use:
The use of xylazine cut into illicit fentanyl is growing. Drug users may not even be aware that the substances they are using contain xylazine, given its lack of unique identifying effects and the fact that it doesn't show up on standard opioid tests. This lack of awareness can lead to unexpected and severe health consequences.
Implications for Detox Providers:
1. Assessment and Testing:
The first step in addressing this problem is recognizing its existence. Detox providers must familiarize themselves with this trend and consider it when assessing patients. This is something to discuss with other providers in your region, as the local drug scene can vary from city to city. While xylazine may not appear on standard urine drug screens, providers should consider sending samples for comprehensive toxicology screens when xylazine use is suspected.
The presence of Xylazine will affect the presentation of both intoxication as well as withdrawal. Below is a table which ought to describe some of the differences to look for:
2. Withdrawal Management:
The presence of xylazine can complicate withdrawal management. As a sedative with a shorter half-life than many opioids, its withdrawal symptoms may emerge more quickly and present differently than typical opioid withdrawal. Providers need to be prepared to recognize and treat these atypical symptoms, such as hypertension and tachycardia.
3. Medical Complications:
The medical complications associated with xylazine, including skin lesions and infections, require particular attention during detoxification. These complications may necessitate more intensive medical management, prolonging the recovery process.
4. Patient Education and Harm Reduction:
Patient education is crucial. Informing patients about the risks associated with fentanyl adulterated with xylazine can be a critical step in the harm reduction process. Encourage patients to use harm reduction strategies, such as never using alone, keeping naloxone on hand, and considering drug testing strips.
5. Broader Intervention Strategies:
Community outreach programs and public health initiatives should be involved to disseminate information about this growing issue. Collaborations with local pharmacies, law enforcement agencies, and other community resources can help raise awareness and provide resources for those at risk.
6. Continual Learning and Adaptation:
Given the rapid evolution of illicit drug use, healthcare providers must stay updated on emerging trends. In addition to speaking with other PMHNPs in your region (which is likely the best bet), participating in professional development activities, attending relevant seminars can help providers stay informed.
Patient Scenario:
John, a 28-year-old man, presented to the detox clinic accompanied by his sister. He was disheveled, had difficulty staying awake during the interview, and had notable skin sores. His sister reported that John had been using opioids for the past few years but had recently shown new and concerning symptoms.
Keep reading with a 7-day free trial
Subscribe to Short Bits for Inquisitive PMHNP's to keep reading this post and get 7 days of free access to the full post archives.